AI in Healthcare: Transforming Medicine with Benefits and Challenges
The Evolution of AI in Modern Healthcare
Artificial Intelligence (AI) has emerged as a transformative force in the healthcare industry, fundamentally altering how medical professionals approach documentation, diagnosis, treatment planning, and revenue cycle management. In its most basic form, AI in healthcare refers to the use of machine learning algorithms, natural language processing, and other computational methods to analyze medical data, automate routine tasks, and support clinical decision-making. One prominent example is Ambience Healthcare’s AI platform, which assists clinicians with pre-visit agenda design and then leverages the patient’s historical Electronic Health Record (EHR) data along with recorded conversations to automate documentation, including clinical notes, after-visit summaries, referral letters, and even suggesting appropriate medical codes. The integration of AI tools into healthcare systems represents a significant shift from traditional manual processes toward more streamlined, data-driven approaches. This technological revolution is not merely about efficiency but also aims to address some of healthcare’s most pressing challenges, including clinician burnout, documentation overload, and the increasing complexity of medical billing. As healthcare systems worldwide grapple with staffing shortages, mounting costs, and growing administrative burdens, AI offers potential solutions that could fundamentally reshape the industry’s operational landscape.
Benefits: Enhancing Efficiency and Clinical Experience
The adoption of AI in healthcare has demonstrated substantial benefits across various operational aspects, particularly in reducing the administrative burden on medical professionals. At St. Luke’s Health System, for instance, clinicians using Ambience’s AI documentation tool reported an average 39% reduction in documentation time during their pilot program. The impact varied based on specialty, schedule, and working style, but many clinicians noted saving hours each day. One physician even reported a remarkable time savings of 20 hours per week on documentation tasks. This dramatic reduction in administrative workload has profound implications beyond mere efficiency. Dr. Devin Laky, a family medicine physician at St. Luke’s, noted that the AI tool eliminated “the perpetual dread of keeping up with documentation,” providing her with “more mental clarity and presence” both at work and at home. As a new mother returning from maternity leave, she credited the ambient AI technology with allowing her to achieve better work-life balance for the first time in her career. Beyond individual clinicians, healthcare executives also recognize AI’s broader potential. According to a survey by Everest Group and Omega Healthcare, 85% of senior healthcare executives believe AI will improve efficiencies in revenue cycle management (RCM) operations over the next five years. This confidence is not based on blind optimism but on direct experience with both the challenges and potential of AI in real-world RCM environments. Healthcare providers are navigating what some executives describe as “a perfect storm of mounting billing complexities, growing patient financial responsibility, staffing shortages and outdated technology systems.” In this challenging context, AI offers practical solutions to longstanding inefficiencies across the revenue cycle continuum, from front-end eligibility verification to back-end denial management.
Beyond Efficiency: Improving Patient Care and Financial Performance
The benefits of AI in healthcare extend well beyond administrative efficiency and directly impact the quality of patient care and health system financial performance. By automating documentation and administrative tasks, AI tools like Ambience’s platform allow clinicians to be more present and engaged during patient visits, enabling patients to feel “more seen and heard.” This enhanced quality of interaction represents a significant improvement in the patient experience, potentially leading to better health outcomes through improved clinician-patient communication and trust. From a financial perspective, AI is increasingly viewed as a strategic investment rather than merely a cost-saving measure. By 2030, AI/machine learning is projected to become the top investment area for revenue cycle management leaders, with 66% citing it as a high priority. This represents a shift from viewing AI as an experimental initiative to recognizing it as “a core enabler of financial performance and patient-centric care” that is becoming “foundational to how healthcare organizations think about resilience, competitiveness and quality outcomes.” The evolution toward “agentic AI” – systems capable of making decisions, planning tasks, and optimizing workflows – represents the next frontier in healthcare automation. These advanced applications have significant potential in areas such as prior authorizations or automated medical coding from clinical narratives, which could further transform healthcare financial strategies as regulatory clarity and technology maturity improve. Early implementations in areas such as eligibility verification, claims analysis, and AI-driven patient communication are already demonstrating tangible improvements in both operational efficiency and accuracy, reducing denials and administrative burden while enhancing patient interactions.
Challenges and Barriers to Implementation
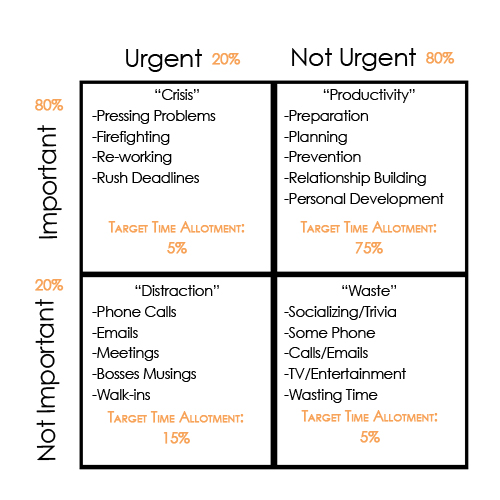
Despite the promising benefits, healthcare organizations face significant challenges in implementing AI technologies effectively. According to survey findings, the most frequently cited barrier to AI adoption – reported by approximately 80% of respondents – is a lack of in-house expertise. Additional obstacles include integration difficulties with legacy electronic health records systems and concerns regarding data privacy and regulatory uncertainty. To overcome these barriers, many healthcare organizations are beginning with proof-of-concept projects, implementing rigorous human-in-the-loop validation processes, and pursuing strategic partnerships to address skill gaps. Some are adopting modular, incremental approaches to EHR integration and leveraging AI as a catalyst for broader information technology modernization. The integration of AI, particularly generative AI, into revenue cycle processes presents unique complexities requiring advanced data science capabilities, secure infrastructure, and regulatory oversight. This complexity explains why many healthcare organizations prefer collaborating with third-party vendors that can provide not only the technology but also the operational support and compliance expertise needed for large-scale deployment. The survey found that 51% of healthcare leaders expect an increase in RCM outsourcing budgets by 2030, reflecting this shift toward strategic partnerships for AI implementation. However, more fundamental concerns exist regarding AI’s appropriateness in certain healthcare contexts. An international team of researchers has called on healthcare AI proponents to be more mindful of the technology’s unsuitability across much of the developing world. The issue isn’t that resource-starved clinics, hospitals, and healthcare systems wouldn’t like to adopt AI and other emerging technologies to improve care, streamline workflows, and optimize administration. Rather, they argue that these facilities would first need help solving much more basic problems. The researchers caution that “Like previous medical technologies, AI tools risk reinforcing existing patterns of technological dependency if implemented without addressing fundamental health system requirements.” This raises important questions about “who benefits from pushing an AI-first narrative for healthcare, and does this paradigm truly serve the interests of the most disadvantaged patients?”
Ethical Considerations and Future Direction
The implementation of AI in healthcare necessitates careful consideration of ethical implications, particularly regarding equity, dependency, and the fundamental requirements of healthcare systems. Building on the work of late infectious disease specialist and humanitarian Dr. Paul Farmer, researchers propose a “5S” framework for evaluating AI’s appropriateness in various healthcare contexts. This framework emphasizes that Staff (healthcare workers must be supported before AI can be considered), Stuff (basic resources and infrastructure must precede technological investment), Spaces (physical healthcare infrastructure cannot be leapfrogged by digital solutions), Systems (strong healthcare governance has to come before innovative technological improvement), and Support (social infrastructure determines healthcare success more than technology) are prerequisites that must be addressed before implementing advanced AI solutions. The researchers argue that “Until healthcare systems can demonstrate sustainable capabilities across all dimensions of the 5S framework, AI implementation runs the risk of not just being premature but potentially harmful.” They maintain that “The measure of success in healthcare should not be the sophistication of our technology but the consistent delivery of quality care to all who need it.” Another significant concern is the potential for AI dependency among healthcare workers. Casey Greene, a biomedical informatics professor at the University of Colorado School of Medicine, emphasizes that remaining mindful of this risk is “absolutely vital.” He notes, “We want to reduce friction but not critical thinking,” acknowledging that humans excel in certain areas and stating, “We want to ensure we’re supporting that and not replacing it.” Healthcare leaders are increasingly recognizing the importance of building trust in AI systems. Steve Miff and Aida Somun, executives at the Parkland Center for Clinical Innovation in Texas, argue that trustworthiness in healthcare AI isn’t achievable without transparency. They note that despite advances in AI applications for clinical decision support and population health, the healthcare industry remains “confronted by our most enduring issues—patient access challenges and resource capacity.” Looking forward, the World Health Organization is working to establish unified standards for AI in healthcare through the United Nations. WHO-affiliated researchers have outlined four priority areas—ethics, regulation, implementation, and operations—which they describe as “foundational in the advancement of equitable, safe and effective AI for the global community.” This global approach to AI governance aims to ensure that as healthcare AI continues to evolve, it does so in a manner that promotes equity, safety, and effectiveness while addressing the diverse capabilities and needs of healthcare systems worldwide.